New Jersey unveils Medicaid overhaul
TRENTON, N.J. (AP) — New Jersey health officials are pushing to tighten the eligibility requirements for new Medicaid enrollees as part of Gov. Christopher Christie's administration's effort to save $300 million by overhauling the health care program for low income and disabled residents.
The proposal would deny coverage to new adult enrollees who earn more than $5,317 per year for a family of three — about one-fifth of the current income requirement. It would also move more participants from fee-for-service plans into managed care and require a $25 copay when hospital emergency rooms are used for non-emergency treatment.
Children would not be affected, but about 23,000 uninsured adults could lose eligibility.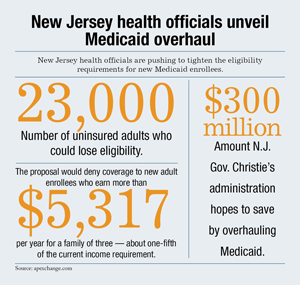
Christie's proposed budget for fiscal year 2012 included a target of $300 million in cuts to Medicaid, but did not detail where the money would come from. Some of those details came Tuesday in an Assembly Budget Committee meeting in which the state's top officials on health and human services presented the framework for a Comprehensive Medicaid Waiver.
The plan by the Republican governor's administration to help alleviate New Jersey's budgetary problems has sparked indignation from Democratic lawmakers who say the state's neediest residents will be denied care, and that having more people uninsured will ultimately be more costly.
"Those 23,000 people are going to get sick this year," said Louis Greenwald, the committee chairman. "Where are you suggesting they're going to go?"
Jointly funded by the federal and state government, Medicaid provides health care services to at-risk populations including the indigent, blind and disabled. Each state sets its own requirements and benefits, but states must apply to the federal government for a waiver before making major changes.
New Jersey's share of the cost of Medicaid adds up to almost $5 billion per year, according to the state. The federal government pays a similar amount to fund the nearly 1.3 million residents enrolled.
"The entire premise of the Comprehensive Medicaid Waiver is to restructure the program from the ground-up," said Human Services Commissioner Jennifer Velez.
Her counterpart in the Department of Health and Senior Services, Mary O'Dowd, told the committee the changes will allow the state to better coordinate care, decrease institutionalization and encourage healthy behaviors.
But lawmakers grilled O'Dowd and Velez about how big a hole the cuts would create in the state's social safety net.
"I'm so very, very troubled by this proposal," said Assemblyman Gary Schaer, a Democrat. "It's not government's role to be charity, but it is government's role to provide opportunity. We're taking it away. They can barely survive now."
Velez cited the state's precarious budget situation and reminded legislators that the proposal doesn't withhold health care from those currently eligible, but simply freezes new enrollment. She said the new copay is intended to encourage fewer residents to use the emergency room for routine care, and pointed out that in true emergencies, nobody is turned away.
Greenwald pointed out the irony that, under the state's plan, residents earning less than $103 per week would be saddled with the copay, while those earning too much to qualify for Medicaid — but not enough to pay their own way — would be treated for free. Health officials haven't presented a specific cost breakdown and only plan to provide cost ranges, which Greenwald said makes it impossible to know whether Medicaid is more expensive than paying for those who present for services without insurance.
"This is not really thought out to the nth degree — and we're losing time," Greenwald said.
The human services commissioner plans to present the waiver to federal authorities June 30. The next day, New Jersey will move residents receiving medical day care services into managed care.
If the Obama administration approves the changes, it wouldn't be the first time New Jersey has curtailed enrollment. In 2001, the state halted enrollment for childless adults, estimated to number around 300,000. That left only those receiving welfare able to get government-funded health care. Additional eligibility reductions took effect in 2002 and 2010.
The fallout from the most recent reduction is the subject of a report being drafted by NJ Policy Perspective, a liberal think tank. Senior Policy Analyst Ray Castro, a former state health official, characterized the Christie plan as abandoning health care for parents in favor of focusing on children, the elderly and disabled individuals.
"If a parent is ill, how could they support that child?" Castro said after the hearing.
But others argue if the governor is to make good on his word not to raise taxes, major cutbacks have to occur somewhere.
"In New Jersey, there's a lot of duplication, which costs a lot of money," said Chris Kniesler, executive director of Solutions for New Jersey, a conservative policy group. "No one's going to go without — people are just going to get it in a different way."
Duplicative medical services are providing fodder for another ongoing skirmish between Christie and the Democratic-controlled Legislature.
On Monday, the state Senate approved a bill restoring $7.5 million in cuts to women's health care programs. Christie, who has already vetoed the measure once, maintains that women already have access to those services through Federally Qualified Health Centers.
___
Josh Lederman can be reached at http://www.twitter.com/joshledermanAP
Children would not be affected, but about 23,000 uninsured adults could lose eligibility.
Christie's proposed budget for fiscal year 2012 included a target of $300 million in cuts to Medicaid, but did not detail where the money would come from. Some of those details came Tuesday in an Assembly Budget Committee meeting in which the state's top officials on health and human services presented the framework for a Comprehensive Medicaid Waiver.
The plan by the Republican governor's administration to help alleviate New Jersey's budgetary problems has sparked indignation from Democratic lawmakers who say the state's neediest residents will be denied care, and that having more people uninsured will ultimately be more costly.
"Those 23,000 people are going to get sick this year," said Louis Greenwald, the committee chairman. "Where are you suggesting they're going to go?"
Jointly funded by the federal and state government, Medicaid provides health care services to at-risk populations including the indigent, blind and disabled. Each state sets its own requirements and benefits, but states must apply to the federal government for a waiver before making major changes.
New Jersey's share of the cost of Medicaid adds up to almost $5 billion per year, according to the state. The federal government pays a similar amount to fund the nearly 1.3 million residents enrolled.
"The entire premise of the Comprehensive Medicaid Waiver is to restructure the program from the ground-up," said Human Services Commissioner Jennifer Velez.
Her counterpart in the Department of Health and Senior Services, Mary O'Dowd, told the committee the changes will allow the state to better coordinate care, decrease institutionalization and encourage healthy behaviors.
But lawmakers grilled O'Dowd and Velez about how big a hole the cuts would create in the state's social safety net.
"I'm so very, very troubled by this proposal," said Assemblyman Gary Schaer, a Democrat. "It's not government's role to be charity, but it is government's role to provide opportunity. We're taking it away. They can barely survive now."
Velez cited the state's precarious budget situation and reminded legislators that the proposal doesn't withhold health care from those currently eligible, but simply freezes new enrollment. She said the new copay is intended to encourage fewer residents to use the emergency room for routine care, and pointed out that in true emergencies, nobody is turned away.
Greenwald pointed out the irony that, under the state's plan, residents earning less than $103 per week would be saddled with the copay, while those earning too much to qualify for Medicaid — but not enough to pay their own way — would be treated for free. Health officials haven't presented a specific cost breakdown and only plan to provide cost ranges, which Greenwald said makes it impossible to know whether Medicaid is more expensive than paying for those who present for services without insurance.
"This is not really thought out to the nth degree — and we're losing time," Greenwald said.
The human services commissioner plans to present the waiver to federal authorities June 30. The next day, New Jersey will move residents receiving medical day care services into managed care.
If the Obama administration approves the changes, it wouldn't be the first time New Jersey has curtailed enrollment. In 2001, the state halted enrollment for childless adults, estimated to number around 300,000. That left only those receiving welfare able to get government-funded health care. Additional eligibility reductions took effect in 2002 and 2010.
The fallout from the most recent reduction is the subject of a report being drafted by NJ Policy Perspective, a liberal think tank. Senior Policy Analyst Ray Castro, a former state health official, characterized the Christie plan as abandoning health care for parents in favor of focusing on children, the elderly and disabled individuals.
"If a parent is ill, how could they support that child?" Castro said after the hearing.
But others argue if the governor is to make good on his word not to raise taxes, major cutbacks have to occur somewhere.
"In New Jersey, there's a lot of duplication, which costs a lot of money," said Chris Kniesler, executive director of Solutions for New Jersey, a conservative policy group. "No one's going to go without — people are just going to get it in a different way."
Duplicative medical services are providing fodder for another ongoing skirmish between Christie and the Democratic-controlled Legislature.
On Monday, the state Senate approved a bill restoring $7.5 million in cuts to women's health care programs. Christie, who has already vetoed the measure once, maintains that women already have access to those services through Federally Qualified Health Centers.
___
Josh Lederman can be reached at http://www.twitter.com/joshledermanAP